Guidance Center to Host 23rd Annual Jonathan Krevat Memorial Golf & Tennis Classic
Roslyn Heights, NY, May 1, 2019 —North Shore Child & Family Guidance Center will be holding its 23rd annual Jonathan Krevat Memorial Golf & Tennis Classic on Monday, June 3, 2019, at the North Hempstead Country Club in Port Washington, one of the region’s premier courses!
Co-chairs Mike Mondiello, Michael Schnepper and Troy Slade are once again working together to create a stellar event filled with friendly competition, delicious dining and wonderful auction prizes. This year, the event is celebrating the dedicated mental health professionals at the Guidance Center— the people who are at the heart of the many success stories of moving families from hurting to healing.
From Left to Right: Troy Slade, Mike Mondiello, Dan Donnelly and Michael Schnepper
“The reason the Guidance Center changes so many lives for the better is because the staff is composed of caring, compassionate and highly trained individuals,” said Slade, who is a member of the Board of Directors. “I’m thrilled that we are celebrating them at this year’s Krevat Cup.”
“This is going to be a phenomenal event,” said Mondiello, also a member of the Guidance Center’s Board of Directors. “The North Hempstead Country is a beautiful course, and we are excited to hold the Krevat Cup at this elegant location for the first time!”
Established on Long Island’s beautiful and serene Gold Coast in 1916, the North Hempstead Country Club features a tree-lined, superiorly manicured golf course designed by renowned architect A. W. Tillinghast, one of the most creative and productive golf course designers ever.
In addition to golf, the event will feature round robin tennis (for the non-golfers among the attendees), a delicious brunch and a gourmet dinner after the day’s games conclude. It will also feature a silent and live auction, with prizes ranging from club seats for a Yankee game to exciting vacation packages and much more.
Dan Donnelly, one of the Guidance Center’s most ardent supporters, as well as a former Krevat Cup honoree, will be serving again as the emcee and auctioneer. “I’m so pleased that this year’s event is celebrating the Guidance Center’s amazing staff,” says Donnelly. “The people working here are such caring souls who are truly devoted to saving lives.”
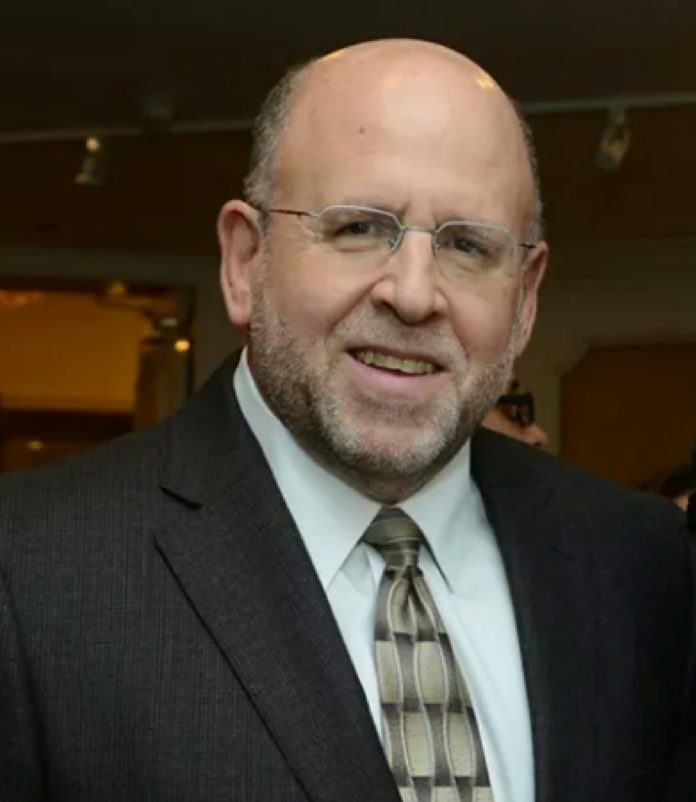
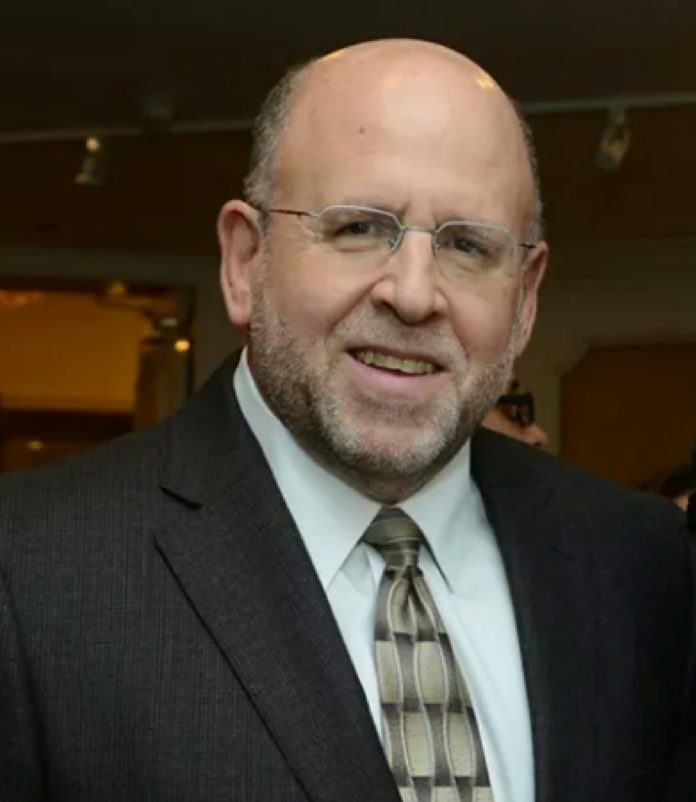
Left to right: Michael Mullman, Ed Geller, Jeff Krevat and Peter Braverman
The other auctioneer for the evening portion of the event is Andrew Marcell, a Guidance Center Board Member. “The Krevat Cup is one of the most enjoyable events of the season,” Marcell said. “It’s a win-win: Everyone has a terrific time while supporting the lifesaving mission of the Guidance Center.”
Andrew Malekoff, Executive Director of the Guidance Center, said, “The event is crucial to our fundraising efforts, and will help us continue to help thousands of children each year who are struggling with issues such as bullying, depression, anxiety and substance abuse.”
Thank you to Fifth Avenue of LI Realty/Americana Manhasset, which has signed on as a Diamond Sponsor.
For those interested in joining a team, attending the dinner, becoming a sponsor or placing a journal ad, it’s not too late! Contact Patrick Madden, pmadden@northshorechildguidance.org, (516) 626-1971, ext. 309.
North Shore Child & Family Guidance Center is the preeminent nonprofit, children’s mental health agency on Long Island, dedicated to restoring and strengthening the emotional well-being of children (from birth to age 24) and their families. For more than 65 years, the Guidance Center has been a place of hope and healing, providing innovative and compassionate treatment to all regardless of their ability to pay.
About Us:
As the preeminent not-for-profit children’s mental health agency on Long Island, North Shore Child & Family Guidance Center is dedicated to restoring and strengthening the emotional well-being of children (from birth – age 24) and their families. Our highly trained staff of psychiatrists, psychologists, social workers, vocational rehabilitation counselors and other mental health professionals lead the way in diagnosis, treatment, prevention, training, parent education, research and advocacy. The Guidance Center helps children and families address issues such as depression and anxiety; developmental delays; bullying; teen pregnancy; sexual abuse; teen drug and alcohol abuse; and family crises stemming from illness, death, trauma and divorce. For more than 65 years, the Guidance Center has been a place of hope and healing, providing innovative and compassionate treatment to all who enter our doors, regardless of their ability to pay. For more information about the Guidance Center, visit www.northshorechildguidance.org or call (516) 626-1971.

“Guidance Center Luncheon Raises Over $87,000,” Blank Slate Media, April 22, 2019

Board members and supporters of the Guidance Center’s lifesaving mission had a wonderful time at this year’s Spring Luncheon.
A sellout crowd of 245 people joined together on Wednesday, April 17 for North Shore Child & Family Guidance Center’s Annual Spring Luncheon. This year’s event, which supports the Guidance Center’s mission to restore and strengthen the emotional well-being of children and their families, was a record-breaker, raising more than $87,000.
The luncheon, which took place at Glen Head Country Club, began with a morning round of mahjong, canasta and bridge, along with unique shopping boutiques from some of Long Island’s trendiest and most charitable small business owners, including Buy the Bag, Club & Country, Dash, I Thrive, Transitions and RFC Fine Jewelry, among others.
After a luncheon buffet, Vanessa McMullen, supervisor at the Guidance Center’s Marks Family Right From The Start 0-3+ Center in Manhasset and also head of the agency’s Diane Goldberg Maternal Depression Program, introduced the day’s speaker, former client Katherine. The audience was completely engrossed as Katherine shared her experience with postpartum depression and talked about the lifesaving treatment she received at the Guidance Center.
She told the crowd, “I was desperately seeking someone who could tell me that I could get through this and convince me that it would get better. When I was finally connected with North Shore Child & Family Guidance Center, my life and my daughter’s life were changed forever… The Guidance Center has not only given me back my life, it has given my family a future.”
“Katherine’s story was incredibly moving,” said Nancy Lane, Guidance Center board president. “When she spoke about the dedication of the Guidance Center staff to both her and her family, I was incredibly proud. Our dedicated team of professionals gives their all to bring hope and healing to each and every client.”
The luncheon couldn’t have been so successful without the hard work of the co-chairs, Jan Ashley, Amy Cantor and Alexis Siegel.
“The enormous success of this year’s event is largely due to the incredible dedication of our three co-chairs,” said Andrew Malekoff, executive director of the Guidance Center. “They have put so much time and energy into the luncheon for several years, and we are truly grateful to them for continuing to make each year more special than the last.”
The Guidance Center is also grateful for the support of its sponsors. They are: Adelphi University, Baxter Smith & Shapiro PC, Amy Cantor, Ruth Fortunoff Cooper, Fara Copell, Linda Cronin, Julie Epstein, Fifth Avenue of LI Realty/Americana Manhasset, Joan & Jeffrey Grant, Janni and Associates/FNA, Deborah Klein, Rosemarie Klipper, Tracey Kupferberg/CBR, NYU Winthrop Women’s and Children’s Services, Raich Ende Malter & Co. LLP, Alexis Siegel, Signature Bank, Ruth & Michael Slade, South Oaks and Zucker Hillside Hospitals — Northwell Health and Carol Wolowitz.
Guidance Center Spring Luncheon Raises Over $87,000
Roslyn Heights, NY, April 22, 2019 — A sellout crowd of 245 people joined together on Wednesday, April 17, 2019, for North Shore Child & Family Guidance Center’s Annual Spring Luncheon. This year’s event, which supports the Guidance Center’s mission to restore and strengthen the emotional well-being of children and their families, was a record-breaker, raising more than $87,000.
The luncheon, which took place at Glen Head Country Club, began with a morning round of Mahjong, Canasta and Bridge, along with unique shopping boutiques from some of Long Island’s trendiest and most charitable small business owners, including Buy the Bag, Club & Country, Dash, I Thrive, Transitions and RFC Fine Jewelry, among others.
After a delicious luncheon buffet, Vanessa McMullen, Supervisor at the Guidance Center’s Marks Family Right From The Start 0-3+ Center in Manhasset and also head of the agency’s Diane Goldberg Maternal Depression Program, introduced the day’s speaker, former client Katherine. The audience was completely engrossed as Katherine shared her experience with postpartum depression and talked about the lifesaving treatment she received at the Guidance Center.
She told the crowd, “I was desperately seeking someone who could tell me that I could get through this and convince me that it would get better. When I was finally connected with North Shore Child & Family Guidance Center, my life and my daughter’s life were changed forever. … The Guidance Center has not only given me back my life, it has given my family a future.”
“Katherine’s story was incredibly moving,” said Nancy Lane, Guidance Center Board President. “When she spoke about the dedication of the Guidance Center staff to both her and her family, I was incredibly proud. Our dedicated team of professionals gives their all to bring hope and healing to each and every client.”
The luncheon couldn’t have been so successful without the hard work of the co-chairs, Jan Ashley, Amy Cantor and Alexis Siegel. “The enormous success of this year’s event is largely due to the incredible dedication of our three co-chairs,” said Andrew Malekoff, Executive Director of the Guidance Center. “They have put so much time and energy into the luncheon for several years, and we are truly grateful to them for continuing to make each year more special than the last.”
The Guidance Center is also grateful for the support of its sponsors. They are: Adelphi University, Baxter Smith & Shapiro PC, Amy Cantor, Ruth Fortunoff Cooper, Fara Copell, Linda Cronin, Julie Epstein, Fifth Avenue of LI Realty/Americana Manhasset, Joan & Jeffrey Grant, Janni and Associates/FNA, Deborah Klein, Rosemarie Klipper, Tracey Kupferberg/CBR, NYU Winthrop Women’s and Children’s Services, Raich Ende Malter & Co. LLP, Alexis Siegel, Signature Bank, Ruth & Michael Slade, South Oaks and Zucker Hillside Hospitals – Northwell Health and Carol Wolowitz.
About Us:
As the preeminent not-for-profit children’s mental health agency on Long Island, North Shore Child & Family Guidance Center is dedicated to restoring and strengthening the emotional well-being of children (from birth – age 24) and their families. Our highly trained staff of psychiatrists, psychologists, social workers, vocational rehabilitation counselors and other mental health professionals lead the way in diagnosis, treatment, prevention, training, parent education, research and advocacy. The Guidance Center helps children and families address issues such as depression and anxiety; developmental delays; bullying; teen pregnancy; sexual abuse; teen drug and alcohol abuse; and family crises stemming from illness, death, trauma and divorce. For more than 65 years, the Guidance Center has been a place of hope and healing, providing innovative and compassionate treatment to all who enter our doors, regardless of their ability to pay. For more information about the Guidance Center, visit www.northshorechildguidance.org or call (516) 626-1971.
“Birth Justice Warriors Fight for Healthy Moms and Babies,” by Andrew Malekoff, L.I. Herald, April 18, 2019
In the modern world we live in, in the richest country in the world and in one of the wealthiest areas of that country, you’d think that Nassau County’s expectant and new mothers, along with their babies, would get the best care in the world.
You’d be wrong — especially when it comes to black women and their babies.
Hackett points to the startling differences between the infant mortality rates in contiguous communities in Nassau. (Infant mortality refers to the death of children before their first birthday.) For example, in Roosevelt there were 8.8 infant deaths per 1,000 births from 2014 to 2016, while neighboring Merrick had a rate of 1 death per 1,000 births. For all of Nassau County, regardless of economic status, the black infant mortality rate is more than four times that of the rate among whites — and even higher than the black infant mortality rate in New York City.
What needs to happen for change to occur in Nassau County, according to Hackett, is the following: 1) inform women after childbirth of warning signs for hemorrhage, embolism or infection; 2) enhance service integration for women and infants; and 3) treat women of color with dignity, respect and culturally relevant care.
Studies show that structural racism is a major factor in disparate infant mortality rates. There is unconscious bias among clinical staff, which negatively perceives black women’s pain before, during and after pregnancy. Even Serena Williams, hardly your average mom, experienced the denial of her concerns by medical professionals during and after the birth of her baby, and it almost led to her death.
Another factor is at work. On a recent NPR broadcast, Tasha Green Cruzat, president of Voices for Illinois Children, cited a study that concluded, “The accumulation of experiences of the African American woman, the racial discrimination that she experiences, produces chronic stress and brings on problems that constitute risk factors for pre-term delivery.”
In March 2018, Hackett and Dr. Nellie Taylor-Walthrust, of the North Shore Child & Family Guidance Center, announced the launch of Birth Justice Warriors, an initiative to train birth advocates to decrease birth inequities. Since the launch, 22 Warriors have been trained. The organizational partners — the Child & Family Guidance Center, Planned Parenthood Nassau County, the March of Dimes, Hofstra’s National Center for Suburban Studies and the Long Island Community Foundation — have provided support and guidance from the beginning, according to Hackett. “Over the past year I have met many strong advocates for black mothers and infants in Nassau County who acknowledge the challenges we face,” she said. “The positive response to Birth Justice Warriors from communities of color tells me that we have tapped into a growing movement for birth equity.”
As the initiative begins its second year, efforts will continue to make injustice visible and raise awareness of black maternal and infant mortality in Nassau by educating medical staff, holding “conversation cafes” with women, partnering with prenatal sites in the county, creating video stories that share the pregnancy and birthing experiences of black women in the county, and making legislative visits to advocate for policy changes to improve birth outcomes.
What can you do? Clearly, there is never a good reason to disrespect someone based on race, sexual orientation, religion — for any reason. But if you are an employer, colleague, physician or neighbor, it is important to understand that a pregnant woman who is disrespected in the workplace or community can develop chronic stress that can lead to miscarriage or the death of an infant. This is disproportionately the experience of pregnant women of color, and it is our moral obligation to remedy this injustice.
Joining up to be a Birth Justice Warrior project is one big way you can make a difference. But whatever you choose to do, awareness, respect and kindness are a great place to start.
Andrew Malekoff is the executive director of North Shore Child & Family Guidance Center, which provides comprehensive mental health services for children and their families, including support for pregnant and parenting teens and their babies. For more, visit www.northshorechildguidance.org.

“A Civil Rights Case for those with Mental Health Issues,” By Andrew Malekoff, Long Island Business News, April 19, 2019
 Last month, a federal court in the Northern District of California found that the giant health insurer United Behavioral Health had been using flawed criteria, contrary to generally accepted standards, to determine medical necessity for the care and treatment of patients with mental health and substance use disorders (MH/SUD).
Last month, a federal court in the Northern District of California found that the giant health insurer United Behavioral Health had been using flawed criteria, contrary to generally accepted standards, to determine medical necessity for the care and treatment of patients with mental health and substance use disorders (MH/SUD).
D. Brian Hufford, a partner at Zuckerman Spaeder, who heads the firm’s health care practice that represented more than 50,000 plaintiffs in the class action lawsuit, commented that “This is a monumental win for mental health patients, who face widespread discrimination in attempting to get the coverage they were promised and that the law requires.”
Why did UBH discriminate? They did it for one reason: to reap the financial rewards that restricting or denying access to outpatient and residential care for individuals living with MH/SUD generates.
Although the finding did not specifically address federal parity law, it does speak directly to the need for far better enforcement of the law.
During the final year of George W. Bush’s administration in 2008, the U.S. Congress passed the Mental Health Parity and Addiction Equity Act (MHPAEA), a federal law to prevent health insurers that provide MH/SUD benefits from carrying out less favorable benefit limits on those benefits than on medical and surgical benefits. In other words, parity law holds that it is illegal to treat diseases of the brain differently than those of any other part of the body.
Chief Magistrate Joseph C. Spero stated that UBH guidelines were aimed first at reducing costs through “an excessive emphasis on addressing acute symptoms and stabilizing crises while ignoring the effective treatment of members’ underlying conditions.”
This decision fires a powerful warning shot at all insurance carriers that cut corners in determining medical necessity without regard for quality of care and with the sole aim of enriching themselves at the expense of their beneficiaries living with MH/SUD.
As plaintiff’s attorney D. Brian Hufford concluded, “For the first time, an insurer was forced to stand trial for denying thousands of mental health and substance use disorder claims, and the court delivered a strong message: what you’re doing is harmful and illegal, and it must end.”
In his decision, Judge Spero found that UBH demonstrated “an abuse of discretion” that was “infected” by monetary incentives intended restrict access to care.
Patrick Kennedy, former US representative and leading mental health advocate, correctly frames the case as a matter of civil rights. He compared the ruling to the landmark 1954 Supreme Court decision that found racial segregation in public schools unconstitutional. He said that the UBH ruling is the Brown v. Board of Education for the mental health movement.
The insurance industry has consistently discriminated against individuals with MH/SUD and with impunity. Government officials, federal and state, have failed to adequately enforce parity law ever since its passage more than 10 years ago.
Now, according to Kennedy, “we have a federal court specifically and forensically breaking down how they get around the federal law. Judge Spero’s decision makes it clear that there will be consequences for disregarding established clinical practice in favor of a financial bottom line.”
Andrew Malekoff is the executive director of North Shore Child & Family Guidance Center.
“How to ‘Be Best’ In Contentious Times,” by Andrew Malekoff, Blank Slate Media, April 16, 2019
Regardless of where you stand in the political spectrum, we can pretty much all agree that these are highly divisive times in our culture.
It often seems that pundits, politicians and people on all sides of the various issues of our day have lost their ability to disagree respectfully. And kids of all ages aren’t immune to absorbing the notion that speaking loudly, aggressively and in a denigrating manner is somehow perfectly acceptable.
In such an environment, how do we teach our kids to approach disagreements without resorting to bullying words and behaviors?
One initiative designed to tackle this problem is First Lady Melania Trump’s “Be Best” campaign. As she states on her website, “It is our responsibility as adults to educate and reinforce to children that when they are using their voices — whether verbally or online they must choose their words wisely and speak with respect and compassion. It remains our generation’s moral imperative to take responsibility and help our children manage the many issues they are facing today, including encouraging positive social, emotional and physical habits.”
Can we really expect political figures to serve as models who live up to the First Lady’s “Be Best” ideal?
In our own backyard, there seems to be a never-ending parade of perp walks, criminal trials, convictions, fines, prison sentences and incarcerations of elected officials for taking bribes, bid-rigging, obstructing justice and more.
Brokering official favors for personal benefit seems to be part of the culture in many political clubhouses, executive offices and legislative chambers in Long Island and New York state. We even see the breakdown in the recent college admission scams, where parents sought preferential treatment for their children through what used to be called payola.
The ideals that Mrs. Trump wants to advance will be more likely to gain traction at home, in school houses, fields of play and or houses of worship. Yet, on occasion an inspiring political leader, super athlete or charismatic musician or actress will touch one’s heart by exuding compassion as they champion meaningful causes such as mental health or drug prevention. They deserve our respect and appreciation for living out the message that people should care about others, not just talking the talk but walking the walk.
Some might say that “Be Best” is an easy phrase to poke fun at, just as “just say no” was during Nancy Reagan’s tenure as first lady, when she launched an anti-drug campaign.
But, as deeply divided as we are becoming as a nation, “Be Best” is a good message. Just because it is a bit corny and not embodied in Washington, D.C., and statehouses across the nation, we should not let our cynicism dilute the message or allow our behavior to dilute the ideal.
To do so would be to turn our back on our kids. If these are times in which we just cannot be best, maybe we can at least strive to be better.
Andrew Malekoff is the executive director of North Shore Child & Family Guidance Center, which provides comprehensive mental health services for children from birth through 24 and their families, including support for pregnant and parenting teens and their babies. To find out more, visit www.northshorechildguidance.org. For more on the Be Best Initiative go to www.whitehouse.gov/bebest.

“Flint Revisited,” by Andrew Malekoff, Anton Media Group, April 12, 2019

(Image by Rudy and Peter Skitterians from Pixabay)
I have protested or testified before government bodies for issues including separating children at the border, school shootings and insurance parity for mental health and substance use disorders. I participated in a number of relief efforts after large-scale disasters such as 9/11 and Hurricane Sandy. Yet nothing haunts me as much as the poisoning of an American city.
The water crisis in Flint, MI, began in April 2014 when, in a cost-cutting measure, the drinking water supply from Detroit’s system was switched to the Flint River. When essential treatment and testing of the water did not follow, health issues ensued.
Government officials turned their backs on the residents of Flint by ignoring the problem that was signaled by foul smelling and discolored water being piped into people’s homes for nearly two years.
Five years later, in January 2019, Gov. Gretchen Whitmer assured Flint residents that they will continue getting free bottled water until all of the pipes are replaced. According to a Jan. 23, 2019 report in The Detroit News, “As of December, the city had replaced nearly 7,000 out of 18,300 lead or galvanized steel water pipes it had identified.”
Beyond the local community, where is the sustained outrage about this unfathomable crime against the children and families of Flint?
I’ve seen a lot in seven decades beginning in the early 1950s, and although I never attempted to rank the horrors over those years, I find the poisoning of Flint, MI, to be among the most troubling. Although there has been backlash, I find it to be muted in comparison to other disasters.
The poisoning of an American city and all of its children, mostly children of color, was a government cost-cutting measure that would have been considered ethnic cleansing by our government leaders if it happened in any other country but our own, according to filmmaker Michael Moore.
To be clear: The residents of an entire American city were poisoned for 19 months. There were warning signs—off-tasting water, body rashes, itchy skin, hair loss—yet government officials told the residents that the water was just fine. It took almost two years of poisoning for the government to wake up after researchers pointed to elevated levels of lead in children.
Corruption in New York State and the country at large is so common that clean government has become an oxymoron. Have we become so inured to it that our attention cannot focus on the latest scandal for very long? Has our capacity for empathy become drained by serial horrors?
If my children were among the poisoned I would likely have to contain feelings of murderous rage, because acting on such impulses would do nothing to help my children.
Yet how do the parents of Flint cope with the knowledge that their children, with still-developing brains, may sustain cognitive impairments that will last a lifetime?
Gov. Whitmer reflected, “Trust was not broken overnight, and it’s not something you can earn overnight.”
The Detroit News reported that “many residents remain wary of the water amid fears that pipe replacement efforts could dislodge lead flakes.” They likely remember that state regulators did not make sure that the city used corrosion control chemicals when it made the switch to the Flint River for its water supply in April 2014.
Will trust ever be restored by parents who understand that their children’s intellectual potential has been compromised by bureaucrats looking for a shortcut to balance the budget? What can one do or say to offer some relief? I cannot think of a thing. Can you?
Andrew Malekoff is the executive director of North Shore Child & Family Guidance Center, which provides comprehensive mental health services for children from birth through 24 and their families. To find out more, visit www.northshorechildguidance.org.

“Kiwanis Presents $1,000 to Guidance Center,” April 10, 2019, Long Island Business News

Kiwanis of North Shore donated $1,000 to support the mission of North Shore Child & Family Guidance Center. (From left) Leslie Kle and Jenna Kern-Rugile.

“Kids First: Child marriage: A widespread and dangerous reality,” The Island Now, April 2, 2019

Did you know that 650 million women and girls alive today were married as children and 12 million girls under 18 are married each year? Globally, around 21 percent of young women were married before their 18th birthday, according to UNICEF.
UNICEF — now called The United Nations Children’s Fund but originally known as the United Nations International Children’s Emergency Fund — was founded in 1946. It was created to offer emergency food and health care to children and mothers in countries that had been devastated by World War II.
I was awakened to this issue while attending the 36th Social Work Day at the United Nations on April 1, 2019. The theme for the day was “Strengthening Human Relationships: Policies and Programs to Protect Children.”
I must confess that I am typically focused on what is happening closer to home, but the information presented by a panel of UN diplomats, policy officers and child protection specialists, as well as front-line social workers, was eye-opening.
In addition to child marriage, the international group of experts focused on a number of other disturbing statistics such as the astounding number of children that are forced into labor from as early as five years old. Worldwide, 218 million children between 5 and 17 years are employed and 73 million work in hazardous conditions
Although the presentations were all compelling, I was particularly interested in how the issue of child marriage manifests itself in the U.S.
The facts are that, although child marriage happens mostly in sub-Saharan Africa, more than 200,000 minors (mostly girls) were married in the United States between 2000 and 2015, and not only in rural areas as is widely believed.
The minimum legal age that young people are permitted to marry in most states in our country is 18, although in six states that age is as low as 14 or 15.
But there are a number of “loopholes,” reported social worker Bushra Husain from NYC-based Sanctuary for Families. For example, if one of the parties is pregnant or if the minor has given birth to a child, then in 47 states, marriage is permitted for children under 18.
Child marriage is a violation of human rights that remains widespread despite laws against it. It can forestall their education and lead to a lifetime of suffering including high rates of domestic violence and the deaths of young adolescent girls due to more complications in pregnancy and childbirth than for women in their 20s.
Furthermore, their children are more likely to be stillborn or die in the first month of life.
The good news is that there is a movement toward change. In 2018, New Jersey and Delaware became the first states to outlaw marriage for anyone less than 18 years of age, with no loopholes.
UNICEF reports that strong bills to end child marriage are currently pending in 11 state legislatures. To learn more about this, go to the link for this special 2018 report by Sarah Ferguson entitled: “What you need to know about child marriage in the U.S.” https://www.unicefusa.org/stories/what-you-need-know-about-child-marriage-us/35059
H.E. Georgi Panayotov, an ambassador to the UN from Bulgaria, tied the day together with a caution by Nelson Mandela: “History will judge us on the difference we make in the everyday lives of children.”
Andrew Malekoff is the Executive Director of North Shore Child & Family Guidance Center, which provides comprehensive mental health services for children from birth through 24 and their families. To find out more, call (516) 626-1971 or visit www.northshorechildguidance.org.

“Shortage Of Psychiatrists Causing A Growing Mental Health Crisis,” CBS New York, April 4, 2019
ROSLYN HEIGHTS, N.Y. (CBSNewYork) – A shortage of mental health providers is keeping some patients waiting for months.
Many families are paying out of pocket to get help because healthcare providers are refusing to take insurance – saying reimbursements are just too low.
One quarter of Long Island families surveyed said they were unable to find a mental health provider who takes their insurance. Those families told CBS2 they’re angered having to wait for help.
“Sometimes it takes them days, weeks, months, even years,” Andrew Malekoff, CEO of North Shore Child & Family Guidance Center said.
Malekoff added the shortage means many families are giving up. Some are enrolling in a “clinics” that lack in privacy or – in Jenna Kern-Rugile’s case – footing the bill for each 45-minute session.
“It was $500 a visit, I was not doing well, I was desperate, but I was willing to pay that because I was desperate… Out of pocket and I wasn’t working because of the depression,” Kern-Rugile explained.
Ninety percent of primary care physicians reportedly accept insurance, but only 55 percent of psychiatrists accept insurance because of the low reimbursement rates.

Fewer and fewer medical students are reportedly going into the field of psychiatry. (Credit: CBS2)
“We are seeing a lot of kids coming in with anxiety depression being diagnosed with ADHD,” Dr. Michele Reed said.
Yet the family practitioner added that she struggles to find psychiatrists for her young patients.
“It’s devastating. Three of the highest burden illnesses for children (are) depression, bi-polar, schizophrenia. Those are the kind of things child psychiatrists treat and there just aren’t enough of us,” psychiatrist Dr. Stephen Perret said.
Major health systems on Long Island are trying to make “behavioral health care” more accessible; placing mental health experts into family care settings where insurance is accepted.
“The last thing you need is to be turned away when you’re calling for help,” Kern-Rugile said.
Experts say medical schools need to graduate 30 percent more students in psychiatric medicine to meet the current demand.

“Shortage of Mental Health Providers Can Leave Patients Waiting Months,” Newsday, April 4, 2019
Many providers don’t take insurance because they say reimbursements are too low, forcing families to pay out of pocket.

Dr. Kristie Golden, an associate director at Stony Brook Medicine, said lower payments from insurers have pushed many medical students to choose fields other than psychiatry, and when providers do not accept insurance not everyone can afford to pay. Photo Credit: Newsday/John Paraskevas
By David Reich-Hale
david.reich-hale@newsday.com
A shortage of mental health professionals has forced some Long Islanders to wait months for an appointment, and patients who do get care without a delay often pay out of pocket because many psychiatrists, psychologists and other therapists don’t take insurance.
Insurance reimbursements for those care providers are too low, and don’t come close to those of several other medical specialties, experts at Long Island’s largest health systems said.
And with demand for treatment high, psychiatrists often only treat patients who can afford to pay out of pocket. That can mean hundreds of dollars for a 45-minute session.

Some providers spend time at lower pay at organizations that help those who can’t pay for care. North Shore Child and Family Guidance Center in Roslyn Heights, led by Andrew Malekoff, is such a service, which operates by raising funds and seeking donors and grants. Photo Credit: Howard Simmons
Nearly 25 percent of respondents in a 2017 survey by Roslyn Heights-based North Shore Child and Family Guidance Center, a not-for-profit children’s mental health agency, said they couldn’t find a single provider who took their insurance.
“What makes the difficulty accessing care particularly difficult for people and families living with mental health and substance-use disorders is that stigma, and the shame it generates leads to delays in their asking for help in the first place,” center executive director Andrew Malekoff said. “Some may wait weeks, months and even years to ask for help.”
In addition, the lower insurance reimbursements have pushed medical students to choose fields other than psychiatry, said Dr. Kristie Golden, associate director of operations at Stony Brook Medicine. Golden said the demand won’t be met unless “psychiatrists come up with ways to make a comparable living and pay off school debt.”
There is also a broader economic cost. Depression and anxiety cost the global economy $1 trillion annually in lost productivity and absenteeism, according to the World Health Organization. But the organization said for every $1 spent on treating those disorders, there is a $4 return in better health and ability to work.
Local health systems are working to improve the situation by opening mental health care centers that accept insurance and locating mental health providers who take insurance within primary-care settings.
However, the shortage of providers is growing. The state Labor Department projected in 2012 that a 25 percent increase in psychiatrists and a nearly 30 percent increase in mental health therapists would be needed to meet demand from 2012 to 2022.
According to the National Alliance on Mental Illness, about 19 percent of adults in the United States, or 43.8 million people, experience some type of mental illness, such as depression, anxiety or bipolar disorder, in a given year. About 21 percent of teenagers experience a severe mental disorder at some point during their life, the group said.

Dr. Michele Reed, a family practitioner in Garden City, says she struggles to find psychiatrists who take the same insurance she does, so it’s difficult for her to send her patients who need help to a psychiatrist. Photo Credit: Newsday/J. Conrad Williams Jr.
Many psychiatrists “who do take insurance come to realize that there isn’t enough time in the day to see patients and then handle all the paperwork, requests and denials that come with taking insurance,” said Dr. Ronald Brenner, chief of behavioral health services for Catholic Health Services in Rockville Centre.
Although regional numbers are hard to come by, the percentage of psychiatrists who don’t take insurance could be higher on Long Island, said Dr. Aaron Pinkhasov, chairman of the Department of Behavioral Health at NYU Winthrop Hospital in Mineola.
“There are more people who could pay out of pocket, so it’s a more feasible option for doctors in a region like this,” Pinkhasov said.

Dr. Stephen Perret, a private child psychiatrist in Westbury, says its “terribly frustrating” not accepting insurance, but the $60 insurance pays for a visit would not cover his costs, which include $200,000 in student loan debt. “The system is a mess,” he says. Photo Credit: Brad Penner
But Long Islanders still have better access than residents of rural areas of New York and the nation, where finding providers is even more difficult, experts said. In metropolitan areas, there are 17.5 mental health providers per 100,000 people, according to an American Journal of Preventive Medicine analysis completed in 2016. The number of providers falls to 5.8 per 100,000 in non-metro counties.
“It’s all perspective, and we are used to an ease of entry, where we don’t need to drive more than 10 minutes to get what we need,” said Janet Kahn-Scolaro, administrative director for behavioral health and family medicine services at South Nassau Communities Hospital in Oceanside. “But even here it could be better.”
Christine Sampson, 37, of Amagansett, said she traveled more than two hours to Hempstead, because she couldn’t find a nearby psychiatrist who took her insurance without a long wait to make an appointment.
“It took me a month just to find a psychiatrist, and he was far away,” she said. “I was desperate, so I did it.”

Patient Christine Sampson had difficulty finding a psychiatrist who would take her insurance on the East End and traveled west for hours for care. She now sees a doctor closer to her home in Amagansett and her co-pay for mental health services is $70. Photo Credit: Veronique Louis
Sampson, who has bipolar disorder, said she now sees a local psychiatrist and therapist, and her six medicines are covered by insurance. Her copay for mental health services is $70.
“One of my medicines would cost $900 without insurance,” she said. “I’m fortunate that on my current insurance, I pay a $40 copay, and that’s it.”
Karen Garcia, 39, of Roslyn said she tried to find mental health treatment.
“I really tried to get therapy, and in every case it was either too pricey or the waiting list was months long,” she said. “I gave up.”
It can be even more difficult to find child psychiatrists who take insurance because there is a shortage of them in general, said Dr. Stephen Perret, who runs a private child psychiatry practice in Westbury.
“We come in to this profession to help people, so it’s terribly frustrating that I can’t take [insurance],” Perret said. “I wouldn’t be able to cover the rent, never mind pay my employees, pay off my $200,000 in student loans or feed my family with the $60 insurance pays for a visit. The system is a mess.”
Sheree Simmons of Brentwood, who is on Medicaid, said she pays $400 to $800 out of pocket every month for her daughter to see a psychiatrist in West Islip. The cost varies, depending on how often she needs to go.
“She also needs more counseling, but I can’t afford it,” Simmons said. “Very few people are taking Medicaid.
She said she calls her daughter “three or four times per day while she is at school to make sure she is all right. It’s all very difficult.”
The lack of providers can also be maddening for family practitioners who can’t find the help needed for their patients, said Dr. Michele C. Reed, who has offices in Garden City and Rosedale, Queens.
“It’s a daily issue,” Reed said. “I routinely see patients, including children, who have anxiety issues. We try to find them a psychiatrist, psychologist, social worker or therapist who can help. But unfortunately we often tell them to call their insurer, because mental health care providers can’t accept what insurers are willing to pay. Also, usually patients who have insurance don’t feel comfortable going to a hospital-based clinic because, more times than not, they don’t feel like they’ll get the same level of privacy and intimacy” that they would in a private practice.
Experts said reimbursements are lower because insurers struggle to quantify the cost for mental health care, which can vary widely for patients with similar diagnoses, depending on the type of treatment. There is also a long-standing lack of recognition that mental illness is as serious as physical illness, and can be tied to other illnesses, they said.
In an effort to make mental health services more accessible, some providers spend time — often at lower pay — at organizations that deliver services to those who can’t pay for care.
For instance, in addition to his private practice, Perret works at the North Shore Child and Family Guidance Center.
“It’s a mission for me, and for others,” he said. “We give whatever we can to help people who need it but can’t afford the care otherwise.”
The center operates by raising between $1.5 million and $2 million a year through fundraising events, individual contributions and grants, executive director Malekoff said.
It accepts all insurance and treats between 5,000 and 6,000 children and their family members yearly, he said. The organization has eight full- and part-time psychiatrists on staff.
“Only through our fundraising are we able to … turn no one away for inability to pay and offer a rapid response with no waiting list,” he said, adding that often families are desperate by the time they seek help.
Major health systems on Long Island are trying to make behavioral health care more accessible.
One strategy includes placing / mental health professionals, sometimes social workers or counselors, inside primary-care practices.
Other systems have opened full-service behavioral health practices that include psychiatrists and psychologists — and take insurance. While psychiatrists are the only ones permitted to write prescriptions, psychologists can handle much of the care patients need, experts said.
South Nassau, which is part of the Mount Sinai Health System, has assigned a psychologist and bilingual social worker to provide behavioral health services at the Center for Primary and Behavioral Care in Hempstead and at a family medical practice in Oceanside. In less urgent cases a primary-care physician can manage the psychiatric medication in collaboration with a psychiatrist, Kahn-Scolaro, at South Nassau, said.
“For patients who require the specialist, the psychiatrist can handle the care directly,” she added.
New Hyde Park-based Northwell Health operates a mental health care office, called Northwell Health Physician Partners Behavioral Health at Manhasset.
“We plan to dot the landscape with this type of practice … They’re in great demand,” said Dr. Blaine Greenwald, Northwell’s vice chairman of psychiatry.
To make it work financially, psychiatrists at the Manhasset office see about 15 to 20 patients daily, and only treat people who need medication as part of their care, Greenwald said.
“The psychiatrist can spend 15 to 30 minutes with a patient without being hurried,” he said. “The practice can’t be financially viable if a psychiatrist spends their time doing psychotherapy too.”
“Therapists see the patients for other services,” he said.
Stony Brook Medicine has embedded behavioral health professionals in various primary-care settings, Golden said.
Stony Brook also uses tele-psychiatry to deliver behavioral health care to patients on the East End, where there are fewer providers to meet the demand.
“It’s easy and convenient for the patients,” Golden said. “A patient goes to a primary-care location and they are seen by a remote behavioral health provider at Stony Brook.”
New York State is expanding telehealth regulations to allow patients to be seen in a variety of locations, including their homes.
But there are federal restrictions that limit the reimbursement of these services to Medicare beneficiaries. A bill that would lift restrictions expired without a vote in 2018.
Catholic Health Services’ Mercy Medical Center operates a behavioral health clinic in Garden City.
“We take everyone, and it can be difficult because it’s overrun,” said Brenner, who is in charge of the health system’s behavioral health care. The facility handled 28,000 visits last year.
Brenner said CHS is also considering opening a clinic in Suffolk.“ “You’d think a clinic would be a profitable enterprise, but given the billing structure, it’s far more complicated, and many clinics struggle,” he said.
NYU Langone this year launched a corporate program in which companies contract directly with the Manhattan-based health system for mental health services.
“We negotiate directly with employers and then provide quality care for a fair level of compensation,” said Dr. Charles Marmar, chairman of the psychiatry department at NYU Langone. “More than 100 behavioral health staff becomes in-network for employees.”
Two large companies have signed on, and others have expressed interest, said Dr. David Ginsberg, the vice chairman of NYU Langone’s psychiatry department.
“It’s a very strong retention tool for companies,” he said.
More than 90 percent of primary care physicians take insurance, while only 55 percent of psychiatrists do.

“North Shore Child & Family Guidance Center Plans Luncheon,” Anton/LI Weekly, April 2, 2019

Board members Andrea Leeds (left) and Ruth Fortunoff Cooper
Are you ready for a fun-filled day of shopping, delicious dining and your favorite games? Then mark your calendars for North Shore Child & Family Guidance Center’s eagerly anticipated annual Spring Luncheon.
This year’s event will be held at the elegant Glen Head Country Club on Wednesday, April 17, from 10 a.m. to 2 p.m. The Clubhouse, which includes a beautiful ballroom, cozy living room area and spacious card room, is the perfect setting for a fun-filled afternoon.
 From left: Co-chairs Amy Cantor, Alexis Siegel and Jan Ashley, with Guidance Center board president Nancy Lane
From left: Co-chairs Amy Cantor, Alexis Siegel and Jan Ashley, with Guidance Center board president Nancy Lane
For those who love to play, the day will open with Mahjong, Canasta and Bridge. Or, if those popular games are not your cup of tea, you can jump right in and start shopping at the unique boutiques, which will feature items from some of Long Island’s trendiest and most charitable small business owners, including Buy the Bag, Club & Country, Dash, I Thrive, Transitions and RFC Fine, among others. The jewelry and apparel are always favorites, but just as chic are the fashionable purses, accessories and housewares. There will also be plenty of opportunities to participate in raffles for luxury prizes, including a $500 gift certificate to Americana Manhasset.
The event will include a fabulous gourmet luncheon featuring the talents of Glen Head Country Club’s master chef.
Registration is now open and sponsorships are available by visiting the Guidance Center’s website, northshorechildguidance.org/spring-luncheon-registration or calling 516-626-1971, ext. 309.
“Explaining High Black Maternal Mortality,” Newsday Letters, By Andrew Malekoff, March 10, 2019
Reader letters to Newsday for Sunday, March 10, 2019.
The assertion by Nassau County Health Commissioner Dr. Lawrence Eisenstein that we do not know the reasons for the high rate of black maternal mortality is just not so [“Addressing the state of black life in Nassau,” News, March 3].
The research on health disparities in maternal and infant mortality speaks to consequences such as the chronic stress of racial and gender discrimination throughout the lives of these women, regardless of socioeconomic status or educational level.
Once we take racism into account, according to policy analysts at the Early Childhood Center for American Progress, “public policy and program solutions must be developed to dismantle it — spurring a lasting impact on health outcomes.”
More concrete steps that can be taken in Nassau County, according to birth equity advocate Martine Hackett of Hofstra University, are to inform women after childbirth of warning signs for hemorrhage, embolism or infection, especially when there are pre-existing conditions; enhance service integration for women and infants; and treat women of color with dignity, respect and culturally relevant care.
Andrew Malekoff, Long Beach
Editor’s note: The writer is executive director of the North Shore Child and Family Guidance Center in Roslyn Heights

“Guidance Center, National Grid Help Prepare Students, for Careers,” Blank Slate Media, March 26, 2019
 Suzanne Martin, Youth Employment Specialist at the Guidance Center (left), with National Grid’s Sarah Kahrs and Paula Gendreau.
Suzanne Martin, Youth Employment Specialist at the Guidance Center (left), with National Grid’s Sarah Kahrs and Paula Gendreau.
North Shore Child & Family Guidance Center and National Grid held the second event in their new partnership as two National Grid employees generously donated their time and expertise to coach students in the Mock Interview Day at Nassau B.O.C.E.S. High School in Wantagh.
At this special annual event, more than 150 interviews were conducted, with employees from National Grid, East Meadow Public Library and other organizations speaking with students individually as if they were on an actual job interview.
“The Mock Interview Day is an invaluable experience for students to practice their communication and social skills,” said Suzanne Martin, youth employment counselor at the Guidance Center’s Intensive Support Program at Nassau B.O.C.E.S., where students receive intensive mental health services on site. “It helps them learn how to present their best selves and realize that first impressions do matter when you’re looking for a job.”
“This event was an incredible experience,” said Sarah Kahrs, U.S. performance excellence coach at National Grid and one of the volunteer interviewers. “It was so exciting to be able to take an active role in helping these young adults prepare for their future. In spite of the students coming in a bit nervous, I was so impressed by how prepared they were.”
Paula Gendreau, National Grid senior supervisor of operations, also enjoyed her experience coaching the students. “Volunteering was such a great opportunity,” she said. “I was impressed by all the positive energy. I was fortunate to meet some great candidates, and it was my pleasure to be a part of a wonderful event.”
Martin said while most of the students were initially very anxious, they felt very accomplished and proud after their interviews. “A lot of students thought they didn’t do well, but they got great feedback from their interviewers,” she said. “It’s a real boost for their self-esteem, and we’re so grateful to National Grid and all the participants for their role in making this event such a huge success.”
The event was the second of several that the Guidance Center has planned in partnership with National Grid. “We work with many organizations across Long Island and in NYC helping to prepare students for their future,” said Kathleen Wisnewski, National Grid customer and community manager. “We’re excited about our partnership with the Guidance Center, and we look forward to more events.”
About North Shore Child & Family Guidance Center:
As the preeminent not-for-profit children’s mental health agency on Long Island, North Shore Child & Family Guidance Center is dedicated to restoring and strengthening the emotional well-being of children (from birth – age 24) and their families.
National Grid is an electricity, natural gas and clean energy delivery company serving more than 20 million people through our networks in New York, Massachusetts and Rhode Island. It is the largest distributor of natural gas in the Northeast.
Guidance Center, National Grid Helps Students Prepare for Future Careers
Volunteers offer their expertise and generosity at annual Mock Interview Day
Roslyn Heights, NY, March 25, 2019 — On March 22, 2019, North Shore Child & Family Guidance Center and National Grid held the second event in their new partnership as two National Grid employees generously donated their time and expertise to coach students in the Mock Interview Day at Nassau B.O.C.E.S. High School in Wantagh.
At this special annual event, more than 150 interviews were conducted, with employees from National Grid, East Meadow Public Library and other organizations speaking with students individually as if they were on an actual job interview.
“The Mock Interview Day is an invaluable experience for students to practice their communication and social skills,” said Suzanne Martin, Youth Employment Counselor at the Guidance Center’s Intensive Support Program at Nassau B.O.C.E.S., where students receive intensive mental health services on site. “It helps them learn how to present their best selves and realize that first impressions do matter when you’re looking for a job.”
“This event was an incredible experience,” said Sarah Kahrs, US Performance Excellence Coach at National Grid and one of the volunteer interviewers. “It was so exciting to be able to take an active role in helping these young adults prepare for their future. In spite of the students coming in a bit nervous, I was so impressed by how prepared they were.”
Paula Gendreau, National Grid Senior Supervisor of Operations, also enjoyed her experience coaching the students. “Volunteering was such a great opportunity,” she said. “I was impressed by all the positive energy! I was fortunate to meet some great candidates, and it was my pleasure to be a part of a wonderful event.”
Martin said that, while most of the students were initially very anxious, they felt very accomplished and proud after their interviews. “A lot of students thought they didn’t do well, but they got great feedback from their interviewers,” she said. “It’s a real boost for their self-esteem, and we’re so grateful to National Grid and all the participants for their role in making this event such a huge success.”
The event was the second of several that the Guidance Center has planned in partnership with National Grid. “We work with many organizations across Long Island and in NYC helping to prepare students for their future,” said Kathleen Wisnewski, National Grid Customer and Community Manager. “We’re excited about our partnership with the Guidance Center, and we look forward to more events.”
Suzanne Martin, Youth Employment Specialist at the Guidance Center (left), with National Grid’s Sarah Kahrs and Paula Gendreau.
About North Shore Child & Family Guidance Center:
As the preeminent not-for-profit children’s mental health agency on Long Island, North Shore Child & Family Guidance Center is dedicated to restoring and strengthening the emotional well-being of children (from birth – age 24) and their families. Our highly trained staff of psychiatrists, psychologists, social workers, vocational rehabilitation counselors and other mental health professionals lead the way in diagnosis, treatment, prevention, training, parent education, research and advocacy. The Guidance Center helps children and families address issues such as depression and anxiety; developmental delays; bullying; teen pregnancy; sexual abuse; teen drug and alcohol abuse; and family crises stemming from illness, death, trauma and divorce. For more than 65 years, the Guidance Center has been a place of hope and healing, providing innovative and compassionate treatment to
all who enter our doors, regardless of their ability to pay. For more information about the Guidance Center, visit www.northshorechildguidance.org or call (516) 626-1971.
About National Grid:
National Grid (LSE: NG; NYSE: NGG) is an electricity, natural gas and clean energy delivery company serving more than 20 million people through our networks in New York, Massachusetts and Rhode Island. We are the largest distributor of natural gas in the Northeast. National Grid also operates the systems that deliver gas and electricity across Great Britain. National Grid is transforming our electricity and natural gas networks with smarter, cleaner and more resilient energy solutions to meet the goal of reducing greenhouse gas emissions by 80 percent by 2050. Our Northeast 80×50 Pathway is an industry leading analysis for how to reach that goal in the states we serve, focusing on the power generation, heat and transportation sectors.
Read more about the innovative projects across our footprint in The Democratization of Energy, an eBook written by National Grid’s U.S. president, Dean Seavers. For more information, please visit our website, follow us on Twitter, watch us on YouTube, friend us on Facebook and find our photos on Instagram.

“The Suburban Myth of Health and Wealth,” U.S. News & World Report, by Gaby Galvin, March 26, 2019
In New York’s Nassau County, a broad portrait of healthy suburbia masks disparities that lie at the local level.
GARDEN CITY, N.Y. – On the surface, Nassau County is a wealthy and thriving suburban enclave in New York City’s backyard.
Home to 1.4 million people and one of two independent counties on Long Island, it’s the picture of community well-being: The area is relatively safe, the unemployment rate is fairly low and most people have health coverage. In U.S. News’ 2019 Healthiest Communities rankings – a project evaluating nearly 3,000 counties across myriad measures of health, housing, economy and more – Nassau County places 96th overall.
That’s the Nassau County many residents know. But further scrutiny reveals stark disparities at the ZIP code level, making it clear that health challenges traditionally thought of as city problems – like pollution, poverty and access to care – can transcend city limits and spill over into suburban rings.
“From the 20,000-foot level, we have one of the wealthiest and healthiest suburbs in America,” says Lawrence Levy, executive dean of Hofstra University‘s National Center for Suburban Studies. “But the closer you get to the ground, the more you realize the unrecognized disparities.
“I am in a community where quality and outcomes in health care are terrific, whereas there are neighborhoods and villages cheek to jowl where you could be in the inner city,” Levy says. “Much of the country (has) fallen victim to this myth of wealth and wellness in the suburbs.”
This longstanding dichotomy can also be found elsewhere: Among America’s 100 most populous metro areas in 2015, more people lived in poverty in the suburbs than in the major cities nearby, according to an analysis presented to Congress by Elizabeth Kneebone, then a senior fellow with the Brookings Institution. A lack of mass transit and fragmented government resources can exacerbate the issue.
But Nassau County – sometimes called the birthplace of post-World War II suburbia – offers a clear example of how a sweeping area assessment can mask neighborhood problems. For example, while census estimates say just 6.2 percentof residents live in poverty, the county’s cost of living is significantly higher than in most of the country, and those struggling to make ends meet have largely been relegated to a handful of neighborhoods.
Community boundaries draw visible lines. In the county hamlet of Merrick, about 88 percent of the approximately 22,000 residents are white, and the median household income is $147,572, according to census estimates. But in neighboring Roosevelt, a 1.77-square-mile hamlet that’s home to a little over 16,000 people, roughly half of public school students are eligible for free or reduced-price lunch, a marker of community poverty. About 98 percent of residents are black or Hispanic.
Half a century after redlining and racial discrimination in housing were banned in the U.S., Nassau County remains one of the most racially segregated of America’s large communities, Healthiest Communities and other data indicate. The legacy of such practices has been documented across the country: Affected communities often lack access to quality housing, jobs, schools and health care, resulting in poorer health outcomes.
“Racial residential segregation is a fundamental cause of health disparities across the board,” says Martine Hackett, an assistant professor and public health researcher at Hofstra University. “If you take that concept – of the outside environment playing a role in the differences on a population level – then the way that looks and presents as the health outcomes of people in suburban areas is going to have a different flavor.”
For example, in Nassau County, black babies are about 3.5 times as likely as white babies to die before their first birthday – a slightly harsher disparity than in New York City, where the poverty rate and uninsured rate are higher. Infant mortality serves as a strong indicator of the health of a population overall, public health experts say, since it’s tied to socioeconomic status, health care access and health care quality – all factors that can be influenced by the structural racism shown to exist in health care.
A community health assessment conducted by the Nassau County Department of Health in 2016 identified nine of the county’s communities, including Roosevelt, as areas where “population pockets are disproportionately burdened with a poorer health status,” which can be borne out by shorter life expectancies, higher disease prevalence and less accessible health care. Some problems vary by neighborhoodand demographics, but taken together, the nine communities generally have significantly higher rates of asthma, type 2 diabetes, liver disease and chronic obstructive pulmonary disease than the rest of the county, according to the assessment.
Sexually transmitted infections also are more prevalent in the nine communities, and Nassau County, combined with neighboring Suffolk County, is one of the only suburban areas in the country to receive federal funding through the Ryan White HIV/AIDS program, authorized in 1990 to provide access to health care for low-income people living with HIV.
Local funding to address such health problems is scarce, however, and while underserved communities in Nassau County have advocated for more attention and resources in recent years, progress has come slowly in some arenas and been stagnant in others.
For example, the county helped pay for programs that supported pregnant teenagers and teenage parents in the village of Westbury for decades. But within the last few years, the county has stopped funding all but one such program – Good Beginnings for Babies – which has seen its funding reduced while need has grown, says Nellie Taylor-Walthrust, who leads the initiative for the North Shore Child & Family Guidance Center, a local counseling agency.
Good Beginnings is now the only program to receive discretionary funding through the health department, which saw its budget slashed by roughly $39 million between 2009 and 2018.
Many school districts also have been hesitant to address mental health and substance use issues among students, Taylor-Walthrust says. “Working with our local community leaders, it’s almost like you have to navigate: Who will listen to what I have to say?” she says. “I think there needs to be a meeting of the minds.”
If historical policies and a clouded view of communities in need have perpetuated some health disparities, Nassau County’s sheer number of villages and public school districts – 56 for roughly 201,000 students – has further fragmented the region, isolating communities that are wealthier, healthier and typically whiter and preventing them from seeing their neighbors’ challenges.
“In my experience, when I point it out to people, they are surprised – all the time – because they had no idea, no realization, even living in these neighborhoods,” Hackett says. “If people don’t know that it’s happening, nobody is going to do anything about it.”
Awareness is a key first step to improving the health of underserved communities, local advocates say, but it’s hardly sufficient.
Northwell Health, the largest hospital system in New York and a major employer in the area, started deploying community interventions to improve health equity in Nassau County in recent years, including by offering “prescriptions” for healthy food to hospital patients who have a diet-related health issue and training community health workers, who are then employed by local organizations and help residents navigate the web of care and services they may need.
“We’ve been seeing there is a gap between where the community is and where social services and health care providers are,” says Nuzhat Quaderi, who manages Northwell’s community health worker program. “We recognize that we’re not the expert in this grassroots, in-the-community work. So how do we build this bridge and create liaisons within the community?”
Dr. Lawrence Eisenstein, Nassau County’s health commissioner, says his health department seeks to provide information and ensure access to services that are available through the region’s many community-based groups, federally qualified health centers, hospitals, school districts and other organizations. The health department also works with the Long Island Health Collaborative – which has roughly 100 community partners across Nassau and Suffolk counties – to compile data, share resources and promote best practices to improve health. The Nassau County Department of Health does not provide clinical services itself.
“It’s all about communication and identifying ways to level the playing field where we see these disparities,” Eisenstein says. “When possible, we try and gear our initiatives toward impacting at-risk communities.”
Still, some advocates have expressed concern about county leaders’ willingness to take on the area’s broader health disparities – and their underlying causes – in a timely and adequate manner. With so many levels of oversight between the county and its dozens of villages, school districts and even water districts, it can be difficult to know who’s responsible for certain issues, creating a “disconnect” between community members and their government leaders, says Jacob Dixon, a community organizer who was born and raised in Roosevelt.
“It’s not to say there’s not the best intentions,” Dixon says. “I think it’s more so: Who is leading the work and who is on the ground to identify there needs to be a larger response? (They) shouldn’t have to come to you to tell you what the problem is, if your job is to come to the people.”
Dixon’s nonprofit organization, Choice for All, was instrumental in having several polluted properties cleaned up in Roosevelt, and worked with the county health department to conduct air and water testing in nearby homes. Now, he is focused on increasing the availability of healthy, affordable food in the area and on improving Roosevelt’s high school graduation rate, which sits at 64 percent.
He also employs two community health workers who were trained through Northwell’s program.
“We have all these different pieces in place, but the concern is sustainability of funding,” Dixon says. Like many community-based groups, many of Choice for All’s initiatives are grant-funded, so when the money dries up, programs can, too.
In the past, Dixon and others have not been able to rely on funding from Nassau County, which is cash-strapped and under the authority of a state financial oversight board despite having one of the highest property tax rates in the state. A report from the county’s comptroller shows Nassau County had more than $3 billion in outstanding long-term debt in 2017, and indicates its financial position was weakened during former County Executive Edward Mangano’s tenure, which ran from 2010 to 2017. (Mangano and his wife recently were convicted on corruption charges.)
County Executive Laura Curran, who took office in 2018, has worked to revamp the county’s property tax system – which a Newsday investigation last year found had disproportionately burdened many property owners under Mangano – and highlighted her plan to regain public trust and ensure financial responsibility during her State of the County address earlier this month.
“We are now on the road to fairness, equity and accuracy,” Curran said during the speech.
Ensuring Nassau County is truly an equitable place to live will require a more targeted focus on health, advocates say. The county is growing more diverse by the year, with census estimates showing an influx of roughly 25,000 Asian and Hispanic immigrants since 2010. Advocates say the county must be willing to change with the population in order to improve health for the people of Nassau County – all of Nassau County.
“Without the ability to dictate from the top, like you can in a city, often these problems are solved one village at a time,” Hofstra’s Levy says. “That’s very inefficient, and not very effective … To break that cycle of dysfunction is very difficult, and it is really the challenge of our time in suburban America.”
“Spring is in the Air as Guidance Center’s Annual Luncheon Returns,” Blank Slate Media, March 18, 2019
Are you ready for a fun-filled day of shopping, delicious dining and your favorite games? Then mark your calendars for North Shore Child & Family Guidance Center’s eagerly anticipated annual spring luncheon.
This year’s event will be held at the Glen Head Country Club on Wednesday, April 17 from 10 a.m. to 2 p.m. The Clubhouse, which includes a beautiful ballroom, cozy living room area and spacious card room, is the perfect setting for a fun-filled afternoon.

For those who love to play, the day will open with mahjong, canasta and bridge. Or, if those popular games are not your cup of tea, you can jump right in and start shopping at the unique boutiques, which will feature items from some of Long Island’s trendiest and most charitable small business owners, including Buy the Bag, Club & Country, Dash, I Thrive, Transitions and RFC Fine, among others. The jewelry and apparel are always favorites, but just as chic are the fashionable purses, accessories and housewares. There will also be plenty of opportunities to participate in raffles for luxury prizes, including a $500 gift certificate to Americana Manhasset.
The event will include a gourmet luncheon featuring the talents of Glen Head Country Club’s master chef.
Registration is now open and sponsorships are available by visiting the Guidance Center’s website, www.northshorechildguidance.org, or calling 516-626-1971, ext. 309.
“Victims of the College Cheating Scandal,” By Andrew Malekoff, Blank Slate Media/the Island Now, March 19, 2019
Every media outlet from Twitter and Facebook to CNN and the New York Times is abuzz with the latest scoop on the college admissions cheating scam.
It’s not surprising that a scandal of this magnitude is big news, but when you add in the fact that well-known celebrities have participated and have even been arrested — well, it’s no wonder that the media and the public are less focused on possible cuts to social security than on this latest frenzy.
Most stories have concentrated on how wealthy parents from Hollywood and beyond used their money and power to have admission tests taken on behalf of their children.
These parents also used an intermediary who created a fake charity to bribe college coaches and other school officials so their kids could apply to schools as recruited athletes, despite the fact that they had little or no athletic ability.
In short, corrupt means were used by parents to gain college admittance to select schools, including some of the most competitive in the nation.
While the stories are largely focused on the parents — especially the famous ones — little has been said about how their actions impact their offspring.
As someone who has spent his entire career working with children and their families, I’m left to wonder: Is there redemption for the student beneficiaries of their parents’ nefarious actions?
It has been presumed, in most if not all cases, that the students were unaware that their parents made payoffs to the schools.
Regardless, there are profound implications for the students that might include them wondering if they have disappointed their parents or failed to live up to their expectations.
I have always been a firm believer that all young people on their path to adulthood are faced with two burning questions: “Will I ever fit in?” and “Will I ever be any good at anything?”
The first question suggests the need for belonging and the second the need for mastery.
Psychiatrist and author Victor Frankl, a Holocaust survivor, spoke about individuals having “the means to live, but no meaning to live for.”
What meaning will the young people that were dishonestly admitted into leading colleges have to live for as the truth really sinks in? How long before a Twitter-storm buries them as they come face-to-face with the reality that everyone belongs on campus but them?
According to Frankl, meaning can be found by being authentic in your interactions with others; giving something back to the world; and changing one’s attitude when faced with a circumstance that you cannot change.
Beyond the bullying of electronic finger pointing, for the young people who were the recipients of the parents’ corrupt largesse, where do they go from here? And, why should we care about them?
I believe we should care because there are lessons to be learned for any child that uncovers and discovers family secrets that leave them wondering what is real in one’s life.
I am going to take a leap to say that the students who gained false admittance to colleges will become demoralized as reality sinks in. Demoralization may include feelings of hopelessness and worthlessness, as well as a sense of alienation and inability to cope.
These kids will need help in developing a reality-based sense of mastery consistent with some experiences of success in the real world.
Rather than seeing them as only privileged and spoiled rich kids, we should root for them to transcend this adversity, which is admittedly not the same as child growing up amid poverty and violence.
Still, we should pull for their lives to find a new and better trajectory than might have emerged from the corrupt actions of their parents.
We all benefit from all our kids’ success.
Andrew Malekoff is the Executive Director of North Shore Child & Family Guidance Center, which provides comprehensive mental health services for children from birth through 24 and their families. To find out more, call (516) 626-1971 or visit www.northshorechildguidance.org.
Spring Is In the Air as Guidance Center Plans Annual Luncheon
Event will feature Mahjong, Canasta, Bridge, great shopping and more
Roslyn Heights, NY, March 18, 2019 — Are you ready for a fun-filled day of shopping, delicious dining and your
favorite games? Then mark your calendars for North Shore Child & Family Guidance Center’s eagerly
anticipated annual Spring Luncheon!
This year’s event will be held at the elegant Glen Head Country Club on Wednesday, April 17 th from 10 a.m.
to 2 p.m. The Clubhouse, which includes a beautiful ballroom, cozy living room area and spacious card room,
is the perfect setting for a fun-filled afternoon.
For those who love to play, the day will open with Mahjong, Canasta and Bridge. Or, if those popular games
are not your cup of tea, you can jump right in and start shopping at the unique boutiques, which will feature
items from some of Long Island’s trendiest and most charitable small business owners, including Buy the Bag,
Club & Country, Dash, I Thrive, Transitions and RFC Fine, among others. The jewelry and apparel are always
favorites, but just as chic are the fashionable purses, accessories and housewares. There will also be plenty of
opportunities to participate in raffles for luxury prizes, including a $500 gift certificate to Americana
Manhasset.
The event will include a fabulous gourmet luncheon featuring the talents of Glen Head Country Club’s master
chef.
Registration is now open and sponsorships are available by visiting the Guidance Center’s website,
www.northshorechildguidance.org or calling 516-626-1971, ext. 309.
About Us:
As the preeminent not-for-profit children’s mental health agency on Long Island, North Shore Child & Family
Guidance Center is dedicated to restoring and strengthening the emotional well-being of children (from birth –
age 24) and their families. Our highly trained staff of psychiatrists, psychologists, social workers, vocational
rehabilitation counselors and other mental health professionals lead the way in diagnosis, treatment,
prevention, training, parent education, research and advocacy. The Guidance Center helps children and
families address issues such as depression and anxiety; developmental delays; bullying; teen pregnancy; sexual
abuse; teen drug and alcohol abuse; and family crises stemming from illness, death, trauma and divorce. For
more than 65 years, the Guidance Center has been a place of hope and healing, providing innovative and
compassionate treatment to all who enter our doors, regardless of their ability to pay. For more information
about the Guidance Center, visit www.northshorechildguidance.org or call (516) 626-1971.

“Schoolyard Bullying Goes Online,” by Andrew Malekoff, Long Island Weekly/Anton Media Group, March 11, 2019
A recent study issued by the Pew Research Center reports that a majority of teenagers (59 percent) have experienced some kind of cyberbullying. The most common forms of harassment cited are name-calling and rumor-spreading.
Other examples of cyberbullying against teens are: receiving explicit messages they didn’t ask for; continuous asking about their whereabouts, what they are doing and who they are with by someone other than a parent; physical threats; and having explicit images of them shared without their permission.
The surveys were completed in 2018 by 743 teens and 1,058 parents living in the U.S. An equal number of boys and girls reported that they were harassed online. The vast majority of teens surveyed believe that online harassment is a problem and do not believe that tech companies, teachers and, least of all, politicians are capable of adequately addressing the problem.
Although New York State has put legal muscle into the fight against bullying in schools with the Dignity for All Students Act, it is not enough to tackle this social problem. No amount of legislation and no penalties for intimidating schoolyard behavior, no matter how severe, can guarantee that children will be safe at all times in, or outside of, school. In fact, the majority of cases that we see at North Shore Child & Family Guidance Center involve anxiety and depression, and of those, a large number of kids and teens report that they are being cyberbullied.
It is no wonder that the teens who responded to the survey rate lawmakers as the least helpful in combating cyberbullying. On May 7, 2018, First Lady Melania Trump launched her “Be Best” campaign to address online behavior and support children’s emotional well-being. Although this is a noble cause that she has chosen to champion, politically-motivated bipartisan cyberbullying among adults has been flooding social media at a frenzied pace. Some incite violence.
For example, most recently, a political consultant who was indicted by a grand jury on a number of charges, including obstructing a congressional investigation, posted a threatening photo on Instagram of the federal judge assigned to his case. The image was of the judge’s face with a rifle scope’s crosshair just above her head.
At the same time teenagers have little faith in adults’ ability to address the problem, they expressed more confidence in parents’ ability to tackle cyberbullying. According to pediatrician Larissa Hirsch, “If you discover that your child is being cyberbullied, offer comfort and support. Talking about any bullying experiences you had in your childhood might help your child feel less alone.” Dr. Hirsch continues by suggesting you should make sure your child understands that he or she is not at fault, and that it reveals more about the bully’s nature than their own.
If you decide to report a case of cyberbullying to your child’s school, be sure to tell your child in advance and develop a plan that is comfortable for both of you. Save or take screenshots of any messages that are threatening as evidence and advise your child not to retaliate as that could lead to an escalation of the situation.
If your child is the bully, Dr. Hirsch recommends, “Talk to your child firmly about his or her actions and explain the negative impact it has on others. Joking and teasing might seem harmless to one person, but it can be hurtful to another.”
Finally, be a good role model by demonstrating positive online habits yourself.
Andrew Malekoff is the Executive Director of North Shore Child & Family Guidance Center, which provides comprehensive mental health services for children from birth through 24 and their families. Visit www.northshorechildguidance.org or call 516-626-1971.
Guidance Center, National Grid Partner, Blank Slate’s Roslyn Times, March 1, 2019
On Feb. 12, North Shore Child & Family Guidance Center and National Grid launched their new partnership with a Career Day talk at the Center for Community Adjustment (CCA), part of Nassau B.O.C.E.S. in Wantagh.
The speaker was Juan Santiago, National Grid Customer and Community Manager, who quickly won over the students with his tale about his life and career journey, from his beginnings as a kid in Brooklyn who shared three pairs of jeans and a bed with his brother and was admittedly not all that interested in school. But he always dreamed big and went for what he called “stretch goals,” and it shows: Santiago’s career trajectory took him from a grocery store bagger to a successful Navy career to a National Grid meter reader and ultimately his current high-level role with National Grid, all while getting his degree online.
He told the students that there are many paths to success, and if they put their hearts and minds to it, they could reach the highest levels.
“Just because someone doesn’t take a traditional route doesn’t mean they are any less motivated,” said Santiago.
When he asked the students what they liked to do, many shared their interests, and he encouraged them to take those passions, make far-reaching goals, and then take the steps needed so that one day, they’d have terrific careers that they’d love.
For example, one student shared that he was good at fixing things, and Santiago told him that his skill could take him to new heights: “Think big. One day you can design and help build a bridge, or maybe you will go to Japan someday and help build the tallest skyscraper. If you can dream it, you can do it.”
Kathleen Wisnewski, National Grid customer and community manager, said that Santiago’s enthusiasm “pulled the kids in and got them engaged from the very beginning.” The kids were “all smiles” by the end of the talk, she added, and many were eager to pull Santiago aside to ask questions and share their own stories.
“While we encourage the exploration and discussion of various tracks to success within the Guidance Center and Nassau B.O.C.E.S., to hear and connect with someone who has navigated the ‘non-traditional’ route to success often leaves more of a lasting impact with our population of students,” said Dena Papadopoulos, mental health counselor at the Center for Community Adjustment (CCA), Nassau B.O.C.E.S, which is one of three B.O.C.E.S schools at which the Guidance Center runs the Intensive Support Program, or ISP. At each school, students who come from all 56 Nassau districts receive intensive mental health services on site.
Suzanne Martin, youth employment counselor at ISP, added, “All the students responded well and enjoyed hearing Juan’s path to success. They found it encouraging and relatable.” She added, “We’re very grateful to Juan and the National Grid team for bringing us this very special program.”
The event was the first of several that the Guidance Center has planned in partnership with National Grid.
“We work with organizations all over Long Island and the city to promote STEM [science, technology, engineering and math],” explained Wisnewski. “We are excited about our new partnership with the Guidance Center, and we look forward to our future events.”
“Waking Up to the Urgency of Mental Health Care,” by Andrew Malekoff, Blank Slate Media, March 5, 2019
Although my daily routine does not include reading Australian news, a social media headline from the Jan. 26, Sidney Morning Herald caught my eye: “Kids are Dying: Calls for Headspace to Publish Waiting Lists.”
Headspace is the name for 110 centers located across Australia that employ mental health and other health professionals to address the health and emotional well-being of young people from ages 12 to 25.
Visits to Headspace, which is funded by the Australian government, are advertised as free of charge. When there is a crisis, they assess risk and formulate a plan in collaboration with the young person seeking help.
Sounds great! So, why the ominous headline? Too many teens in crisis are on Headspace’s waiting lists, which run up to three months. Many have given up hope. Tragically, some are becoming statistics in Australia’s climbing suicide rate.
“Every time a young person in crisis was turned away,” says Headspace Chief Executive Jason Trethowan, it puts them another step closer to “pushing them over the edge.”
Jumping from Australia to the United Kingdom, on Oct. 8, 2018, The Guardian reported that the Royal College of Psychiatrists surveyed 500 diagnosed mental health patients and discovered that some had waited up to 13 years to get the care they needed.
One 20-year-old woman with a history of childhood trauma responded to the survey by stating it took her eight years, until the age of 15, to get treatment. “I was suicidal, but no one would help me. I kept asking for help, and kept being pushed away. Either I wasn’t ill enough to meet the threshold for services, or the waiting list was simply too long,” she noted.
In the U.S., it is too-often the same demoralizing story about disenfranchised youth on waiting lists who end up in hospital emergency rooms that lack adequate psychiatric personnel. For a child survivor of trauma, an ill-equipped ER waiting room often becomes a trigger as opposed to a respite.
Increasingly, economic realities have pushed mental health clinics in the New York metropolitan area to fill the ranks of their staff with fee-for-service workers who carry overflowing caseloads of Medicaid patients. Those patients are seen back to back at 30-minute intervals, factory-style.
At North Shore Child & Family Guidance Center, 20 percent of all admissions come to us as crisis situations, including kids who talk and act as if they don’t want to live. Or, they have endured such trauma in their short lives that they have ceased to function well at home and school. We guarantee to see such emergency cases within 24 to 48 hours — and we don’t kick them out the door after 30 minutes.
Steps are taken to evaluate and reduce the level of risk right from the start to prevent traumatic ER trips. It takes a mission-driven, salaried workforce to get this done properly.
We are pleased that referral sources such as schools and pediatricians understand that we are readily available to all families regardless of income and that they will be evaluated and assigned care rapidly. This is no easy task — certainly not one that can happen in conveyor-belt-style every half hour on the half hour.
Although time is of the essence in the case of an emergency, triage is a thoughtful process that cannot be rushed. Distinctions are made. For example, there is a difference between a high-level emergency involving a child with suicidal thoughts and few if any social supports; and an urgent situation with a child that is verbalizing suicidal feelings, but who is participating in activities, speaking with parents, attending school and clearly has no intent or plan to take his or her life.
In both situations, a careful assessment is needed to understand the level of risk in order to counsel the family accordingly. It is life-and-death work. There are no shortcuts. A dedicated team of salaried professional staff is essential. Yet such places are in short supply.
The Headspace headline — “Kids are Dying” — falls on deaf ears when it comes to mental health care. Someone advised me that if you want to shake things up, you need to examine why you are awake and how you just relate to those who are asleep. One mom carried the ashes of her deceased teenage son to a legislative hearing to awaken the slumbering legislators.
It shouldn’t take ashes to ask for help.
Andrew Malekoff is the executive director of North Shore Child & Family Guidance Center, which provides comprehensive mental health services for children from birth through 24 and their families. To find out more, call 516-626-1971 or visit www.northshorechildguidance.org.
“Waking Up to the Urgency of Mental Health Care,” by Andrew Malekoff, Blank Slate Media, March 5, 2019
Although my daily routine does not include reading Australian news, a social media headline from the Jan. 26, Sidney Morning Herald caught my eye: “Kids are Dying: Calls for Headspace to Publish Waiting Lists.”
Headspace is the name for 110 centers located across Australia that employ mental health and other health professionals to address the health and emotional well-being of young people from ages 12 to 25.
Visits to Headspace, which is funded by the Australian government, are advertised as free of charge. When there is a crisis, they assess risk and formulate a plan in collaboration with the young person seeking help.
Sounds great! So, why the ominous headline? Too many teens in crisis are on Headspace’s waiting lists, which run up to three months. Many have given up hope. Tragically, some are becoming statistics in Australia’s climbing suicide rate.
“Every time a young person in crisis was turned away,” says Headspace Chief Executive Jason Trethowan, it puts them another step closer to “pushing them over the edge.”
Jumping from Australia to the United Kingdom, on Oct. 8, 2018, The Guardian reported that the Royal College of Psychiatrists surveyed 500 diagnosed mental health patients and discovered that some had waited up to 13 years to get the care they needed.
One 20-year-old woman with a history of childhood trauma responded to the survey by stating it took her eight years, until the age of 15, to get treatment. “I was suicidal, but no one would help me. I kept asking for help, and kept being pushed away. Either I wasn’t ill enough to meet the threshold for services, or the waiting list was simply too long,” she noted.
In the U.S., it is too-often the same demoralizing story about disenfranchised youth on waiting lists who end up in hospital emergency rooms that lack adequate psychiatric personnel. For a child survivor of trauma, an ill-equipped ER waiting room often becomes a trigger as opposed to a respite.
Increasingly, economic realities have pushed mental health clinics in the New York metropolitan area to fill the ranks of their staff with fee-for-service workers who carry overflowing caseloads of Medicaid patients. Those patients are seen back to back at 30-minute intervals, factory-style.
At North Shore Child & Family Guidance Center, 20 percent of all admissions come to us as crisis situations, including kids who talk and act as if they don’t want to live. Or, they have endured such trauma in their short lives that they have ceased to function well at home and school. We guarantee to see such emergency cases within 24 to 48 hours — and we don’t kick them out the door after 30 minutes.
Steps are taken to evaluate and reduce the level of risk right from the start to prevent traumatic ER trips. It takes a mission-driven, salaried workforce to get this done properly.
We are pleased that referral sources such as schools and pediatricians understand that we are readily available to all families regardless of income and that they will be evaluated and assigned care rapidly. This is no easy task — certainly not one that can happen in conveyor-belt-style every half hour on the half hour.
Although time is of the essence in the case of an emergency, triage is a thoughtful process that cannot be rushed. Distinctions are made. For example, there is a difference between a high-level emergency involving a child with suicidal thoughts and few if any social supports; and an urgent situation with a child that is verbalizing suicidal feelings, but who is participating in activities, speaking with parents, attending school and clearly has no intent or plan to take his or her life.
In both situations, a careful assessment is needed to understand the level of risk in order to counsel the family accordingly. It is life-and-death work. There are no shortcuts. A dedicated team of salaried professional staff is essential. Yet such places are in short supply.
The Headspace headline — “Kids are Dying” — falls on deaf ears when it comes to mental health care. Someone advised me that if you want to shake things up, you need to examine why you are awake and how you just relate to those who are asleep. One mom carried the ashes of her deceased teenage son to a legislative hearing to awaken the slumbering legislators.
It shouldn’t take ashes to ask for help.
Andrew Malekoff is the executive director of North Shore Child & Family Guidance Center, which provides comprehensive mental health services for children from birth through 24 and their families. To find out more, call 516-626-1971 or visit www.northshorechildguidance.org.
“Breaking the Stigma of Depression,” By Andrew Malekoff, Long Island Herald, February 28, 2019
I’ve been working in the field of children’s mental health for more than 45 years, most of them with the North Shore Child & Family Guidance Center, the leading children’s mental health agency on Long Island, where we turn no one away for inability to pay.
During the early months of each year, we conduct an informal study in an attempt to understand who is calling us for help and what needs they’re calling us about. In recent years, the trend has been that most of the children and teens we see are experiencing anxiety and depression. According to studies, more than 1 in 20 American children and teens have anxiety or depression.
It’s normal in stressful situations to experience anxiety, but some young people have anxiety that interferes with everyday functioning at home or in school. As for depression, while everyone can have a bad day or two that eventually passes, with serious depression there is a more intense and prolonged feeling of hopelessness and inability to function in the important areas of one’s life, at school, at home or with peers.
Some of the signs of clinical depression are feelings of sadness, emptiness, hopelessness, anger or frustration. You no longer care about activities that you typically enjoy; you may not be able to fall asleep, or you sleep longer than usual; you’re often tired; you experience feelings of worthlessness and guilt; and you can’t concentrate or easily make decisions.
Bruce Springsteen, who has opened up about his depression and suicidal thoughts, described it this way in an interview with Esquire: “I once got into some sort of box where I couldn’t figure my way out and where the feelings were so overwhelmingly uncomfortable.”
Depression in teens is widespread: Research indicates that one of every four adolescents will have an episode of major depression during high school, with the average age of onset 14. Sadly, only 30 percent of depressed teens receive treatment, despite the fact that suicide is the third-leading cause of death for young people ages 15 to 24. In fact, according to suicide.org, teen suicides have risen dramatically in recent years.
Why are 70 percent of depressed teens not receiving professional mental health care? One reason is that stigma and shame have the effect of marginalizing and isolating those living with depression. The other reason is that families that seek care for depressed loved ones have trouble accessing professional help, with fewer and fewer providers accepting health insurance.
Despite a federal law that requires health insurers to maintain full rosters of providers — the Mental Health Parity and Addiction Equity Act of 2008 — they often fall short. In addition, the government has failed to adequately enforce the law.
In a 2018 research study by the North Shore Child & Family Guidance Center called Project Access, of the 650 people surveyed, almost half said it was more difficult to find help for mental health or substance use problems than for other illnesses, especially when they were in crisis. Almost 40 percent said their insurance company didn’t have an adequate number of providers, and two-thirds said their insurance company wasn’t helpful when it came to finding care.
There is good news: Anxiety and depression can be treated. Individual and group therapy and, when needed, medication can help. But first you have to be able to find help.
Beyond professional help, how we relate to our loved ones, friends and neighbors living with depression can make a real difference. When we stigmatize someone living with depression, we act as if they have a character flaw or lack of willpower and are undeserving of support. It’s only when we begin to view illnesses above the neck the same as illnesses below it, like cancer or diabetes, that we can reach out and connect rather than further marginalizing and isolating. Sometimes a simple, “How’re you doing? I see you’ve been feeling down. Just know that I’m here for you” can make all the difference.
You can’t instantaneously cure depression, but genuine support and unconditional love can make all the difference in the world for someone living with a mental illness.
Lady Gaga, another artist who has opened up about mental illness, called suicidal thoughts a “spell.” She explained, “We have to have empathy. Be kind, and help each other break the spell and live and thrive.”
Andrew Malekoff is the executive director of the North Shore Child & Family Guidance Center, which provides comprehensive mental-health services to children from birth through age 24 and their families. To find out more, visit www.northshorechildguidance.org.



