by North Shore Child & Family Guidance Center | May 13, 2021 | Anton Media, In The Media
On Tuesday, May 4, you can do good while shopping for some of the finest goods around as North Shore Child & Family Guidance Center hosts “Care for Kids: Spring Shopping Spree.” Many of Roslyn Village’s best stores will be donating a portion of the day’s proceeds to the Guidance Center, Long Island’s premiere children’s mental health nonprofit organization.
As of April 21, the stores participating in the event are: Jill Scherer Ltd., Katherine Tess, Shag New York and Transitions, but the Guidance Center expects the list to grow significantly leading up to the May 4 event.
Leslie Cohen, owner of Transitions, has been a Guidance Center supporter for several years.
“The organization is easy to get behind and support, especially this year, with so many children being affected by the pandemic,” Cohen said. “Having a safe place to help the children cope is wonderful.”
She added that the Spring Shopping Spree will be “a feel-good day.”
According to Ann Corn, owner of Shag New York, nothing is more important than the health of our children.
“Mental health issues do not discriminate by race or financial backgrounds,” she said. “Shag is especially proud to be part of this fantastic fundraising day for the Guidance Center. We are honored to be involved with this amazing organization.”
Alexis Siegel, a member of the Guidance Center’s Board of Directors, expressed the agency’s gratitude for the generosity of participating Roslyn store owners.
“We are all so lucky to live in an area where our businesses and community members are so philanthropic,” Siegel said. “They understand the importance of supporting our work to bring hope and healing to kids and families who are struggling with issues such as depression and anxiety during these incredibly challenging times.”
Shoppers can visit the Guidance Center booth outside of Shag to take part in a raffle that will include many exclusive items.
For more information about the event, contact the Guidance Center at 516-626-1971, ext. 320.

by North Shore Child & Family Guidance Center | May 7, 2021 | Blog
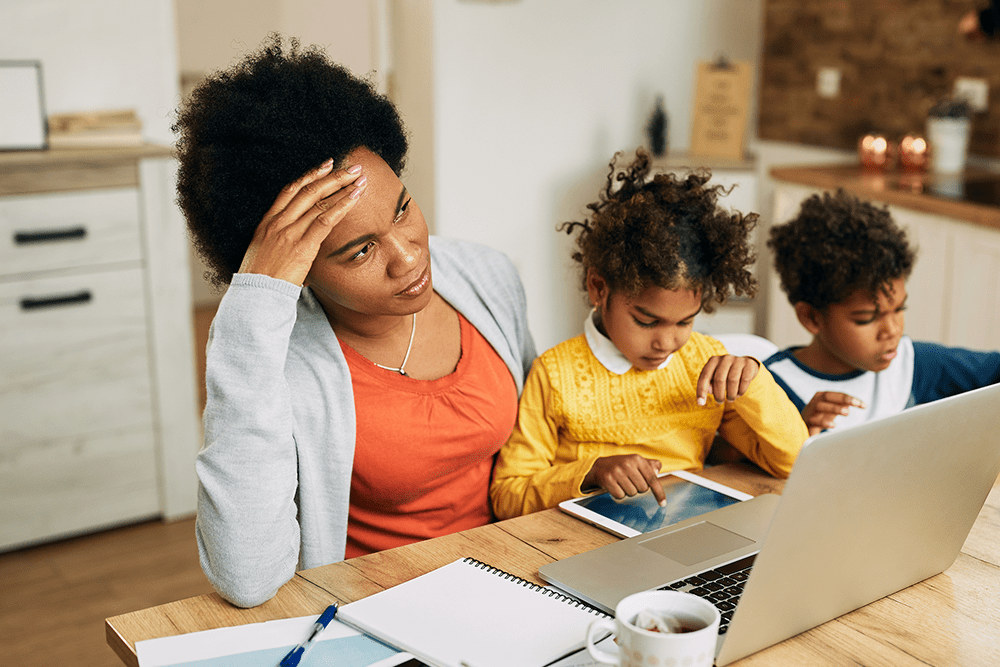
Temper tantrums, “talking back” and other forms of acting out are a normal part of a child’s development. When a youngster is feeling, tired, stressed, upset or out of sorts for any reason, these behaviors aren’t uncommon. Ask any parent!
But when a child’s words and actions cause serious problems at home, school or with peers, they may be diagnosed with a condition known as Oppositional Defiant Disorder, or ODD, a condition that takes a huge toll on family relationships.
“It’s not unusual for children to express their frustrations by losing their tempers or testing your limits by disobeying rules,” says Dr. Sue Cohen, Director of Early Childhood and Psychological Services at North Shore Child & Family Guidance Center. “But when it becomes a pattern of being uncooperative and hostile toward you, their siblings and peers, and other authority figures in such a way that it impacts their daily functioning, it may require professional intervention.”
A diagnosis of ODD is made when behaviors are extreme and go on for at least six months.
According to the American Academy of Child & Adolescent Psychology, symptoms of Oppositional Defiant Disorder may include:
- Frequent temper tantrums
- Excessive arguing with adults
- Often questioning rules
- Active defiance and refusal to comply with adult requests and rules
- Deliberate attempts to annoy or upset people
- Blaming others for his or her mistakes or misbehavior
- Often being touchy or easily annoyed by others
- Frequent anger and resentment
- Mean and hateful talking when upset
- Spiteful attitude and revenge seeking
Signs of ODD typical arise during preschool year, though it can develop later (though usually before early adolescence). Experts aren’t sure what causes ODD, but say that biological, psychological and social issues may play a role. While extreme forms of parenting—too lax or too harsh— may contribute to ODD, that isn’t always the case.
“Parents may feel guilty when their child has ODD, but there are so many unknowns,” says Cohen. “Often one child in the same family has ODD, while other siblings may not. What’s important is getting help, especially since other issues such as attention-deficit hyperactivity disorder (ADHD), learning disabilities, bipolar disorder, depression and anxiety disorders may be present.”
Treatment for ODD can include a variety of therapeutic methods, such as teaching the child anger management and communication techniques, impulse control and problem-solving skills. Including the family in the treatment plan is important, as parents need to develop skills to manage their child’s behavior.
Also, medications may be appropriate, which can be determined in a review with a psychiatrist or other psychiatric professional.
To learn if your child may have ODD, or to get help with other issues that are negatively impacting the life of your child, teen or family, contact the Guidance Center at (516) 626-1971.
How Parents Can Help Children With ODD:
Some helpful tips from the American Academy of Child & Adolescent Psychology:
- Always build on the positives, give the child praise and positive reinforcement when s/he shows flexibility or cooperation.
- Take a time-out or break if you are about to make the conflict with your child worse, not better. This is good modeling for your child. Support your child if s/he decides to take a time-out to prevent overreacting.
- Pick your battles. Since the child with ODD has trouble avoiding power struggles, prioritize the things you want your child to do. If you give your child a time-out in his room for misbehavior, don’t add time for arguing. Say “your time will start when you go to your room.”
- Set reasonable, age-appropriate limits with consequences that can be enforced consistently.
- Maintain interests other than your child with ODD, so that managing your child doesn’t take all your time and energy. Try to work with and obtain support from the other adults (teachers, coaches, and spouse) dealing with your child.
- Manage your own stress with healthy life choices such as exercise and relaxation. Use respite care and other breaks as needed.
Sources:
www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Children-With-Oppositional-Defiant-Disorder-072.aspx

by North Shore Child & Family Guidance Center | May 6, 2021 | In The Media, Newsday
“It’s a fun way to relax,” said Gwen, of Locust Valley. “It’s almost like a therapy, to sit down and do some artwork.”
Gwen wanted children on Long Island to have the same opportunity to unwind and express themselves creatively. They just needed the supplies to do it.
So once again heading to Michael’s, Gwen bought watercolor paints, paintbrushes, colorful pencils, markers, paper and yarn. She’s assembled 175 art kits and donated them to the North Shore Child and Family Guidance Center in Roslyn Heights, a not-for-profit children’s mental health agency.
Gwen made four different versions of the kit, distributing the supplies where they each fit. The “watercolor and Impressionism kit” contained a lesson plan on painter Claude Monet and a brief history of Impressionism. The “mixed medium kit” had a picture of an owl to be colored in and an inspirational quote.
The “collage kit” included facts on artist Pablo Picasso. The most recent kit she’s made contained a canvas, acrylic paint, a paint brush, painter’s tape and a Sharpie pen, so that kids can create geometric shapes.
“I remember coloring as a kid was so much fun to do in art class,” said Gwen. Now, she prefers collaging and painting.
“I wanted to merge both what I liked to do when I was younger, and what I like to do now, and make it good for the younger age group,” she said.
When she first started putting the kits together, Gwen envisioned giving them to children. When she was done, she realized that may not be her only audience.
“Really, any age could do it,” she said. “Any age could have fun with this.”
The North Shore Child and Family Guidance Center serves clients from birth to age 24, according to its website. It provides services that address mental health for children and their families throughout Nassau County, said Lauren McGowan, the director of development. That includes programs on suicide prevention, depression and anxiety, specifically geared toward youth.
Dr. Sue Cohen, the director of early childhood and psychological services, is excited for her clients in particular to use the art kits. Her young clients don’t always have the words to communicate their emotions — that’s where art comes in, Cohen said. Anger can be expressed by scribbling, and fear by drawing what the monster under the bed looks like.
“We use art as a therapeutic tool,” she said. “It’s a great icebreaker to begin to establish rapport with children.”
Cohen added that the art kits arrived at a perfect time for the center: the clinicians had just begun to discuss a safe transition back to in-person therapy sessions and interactive programs, including details such as how to keep crayons and markers clean.
“These individual kits [Gwen] made are perfect because each kit has their own pens, markers and paints,” Cohen said. “As the kids are coming in, they can have a bag designated with their own art supplies, and they can keep them in the office for continued use or take it home.”
McGowan said she’s “delighted” that Gwen has taken initiative and was thoughtful in her approach to helping the center.
“It’ll help our clinicians to communicate better, because kids will open up as they start to feel comfortable and as they’re drawing,” she said. “Art is another modality they can have in their own toolbox, so she’s really given us a gift in that way.”
Gwen dropped off 150 art kits on April 8, and 25 more on April 29. This was a labor of love for her — as she carefully crafted each kit, she said she daydreamed of the moment that she would finally donate them and offer children the same creative outlet that’s helped her through the pandemic.
“Finally getting to hand them over was so exciting,” she said. “I’m excited to be making some more.”
She’s still brainstorming ideas for different art kit themes. McGowan said Gwen’s motivation aligns with the center’s mission to help children in need.
But Gwen’s biggest hope is that children will see that you don’t necessarily have to be a great artist to create something beautiful.
“I hope that younger kids can realize that everybody can be creative and everybody can have fun with art,” Gwen said. “It’s not such a serious thing; you can do whatever you want. It’s something anyone can do and have fun with.”
Click to watch the video interview
Gwen Jones, 17, recently put together 175 art kits and donated them to the North Shore Child and Family Guidance Center in Roslyn Heights. Her hope is that children can use art as an outlet to express themselves, just like she did throughout the coronavirus pandemic. Credit: Howard Schnapp: Photo credit: Peter M. Budraitis Photography
By Rachel Weiss, Rachel Weiss joined Newsday in 2016. She writes and produces local content for newsday.com, including stories on religion and colorful characters from Long Island.

by North Shore Child & Family Guidance Center | Apr 30, 2021 | Blank Slate Media, In The Media
On Tuesday, May 4, you can do good while shopping for some of the finest goods around as North Shore Child & Family Guidance Center hosts “Care for Kids: Spring Shopping Spree.”
Many of Roslyn Village’s best stores will be donating a portion of the day’s proceeds to the Guidance Center, Long Island’s premiere children’s mental health nonprofit organization.
As of April 21, the stores participating in the event are: Jill Scherer Ltd., Katherine Tess, Shag New York and Transitions, but the Guidance Center expects the list to grow significantly leading up to the May 4th event.
Leslie Cohen, owner of Transitions, has been a Guidance Center supporter for several years.
“The organization is easy to get behind and support, especially this year, with so many children being affected by the pandemic,” said Cohen. “Having a safe place to help the children cope is wonderful.”
She added that the Spring Shopping Spree will be “a feel-good day!”
According to Ann Corn, owner of Shag New York, nothing is more important than the health of our children. “Mental health issues do not discriminate by race or financial backgrounds,” she said. “Shag is especially proud to be part of this fantastic fundraising day for the Guidance Center. We are honored to be involved with this amazing organization.”
Alexis Siegel, a member of the Guidance Center’s Board of Directors, expressed the agency’s gratitude for the generosity of participating Roslyn store owners. “We are all so lucky to live in an area where our businesses and community members are so philanthropic,” said Siegel. “They understand the importance of supporting our work to bring hope and healing to kids and families who are struggling with issues such as depression and anxiety during these incredibly challenging times.”
Shoppers can visit the Guidance Center booth outside of Shag to take part in a raffle that will include many exclusive items.
For more information about the event, contact the Guidance Center at (516) 626-1971, ext. 320.